Urology Research: Use of Office-based Urethral Dilation to Treat Women
Author:
Kevin Wood, MS; Wei Chen Lin, MS; Daniel Lee, MD, MS
The following real-world data analysis of the American Urological Association AUA Quality Registry (AQUA) was featured in the June 2022 issue of AUANews. More real-world urologic research leveraging the AQUA network of more than 2,000 healthcare providers, nearly 8 million patients, and 8 years of longitudinal data can be found here.
Trends in Utilization of Office-Based Urethral Dilation for Women: An AQUA Registry Analysis
By: Kevin Wood, MS; Wei Chen Lin, MS; Daniel Lee, MD, MS
Urethral stricture disease in women is rare, accounting for about 0.1-1% of women with voiding complaints.1,2 Urethral dilation has been historically used as a possible treatment for women with various lower urinary tract symptoms such as urgency, frequency, overactive bladder or bladder pain,3,4 despite questionable evidence to support its use for these indications.2,5 Some previous studies found that urethral dilations for women occurred frequently, at almost the same rate as for men despite lower rates of urethral strictures.2 In cooperation with Verana Health, we sought to evaluate how utilization of office-based urethral dilations in women have changed over time. Using the AUA Quality (AQUA) Registry, we measured the rate of office-based urethral dilations performed in women with diagnoses of urethral stricture, overactive bladder, urinary frequency, urgency, interstitial cystitis, and recurrent urinary tract infections. We evaluated patients seen from January 2014 to March 2022.
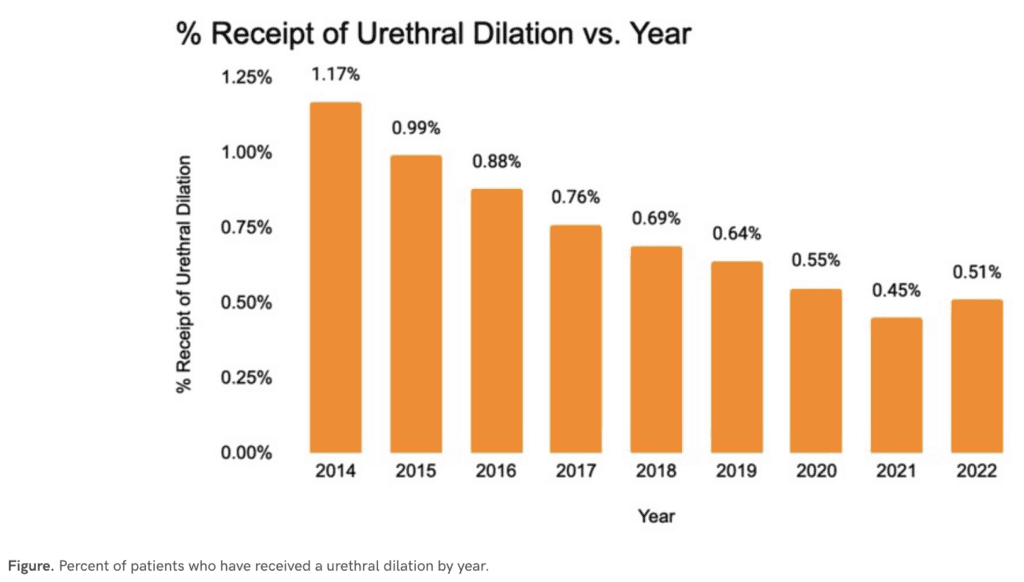
Over the 8 year period, 888,708 women were seen in an AQUA participating urology practice, with urethral stricture disease or diagnoses including interstitial cystitis, recurrent urinary tract infections or lower urinary tract symptoms. There were 6,309 patients (0.7%) who underwent a urethral dilation. Among these women, 79% underwent a dilation for a urethral stricture, while the rest underwent a dilation without a diagnosis of urethral stricture. Of women who had urethral dilations, 51% had repeat urethral dilations within 12 months. Women undergoing urethral dilations were older (median age 68 vs. 64 years) and more likely to be Caucasian (69.6% vs. 59.8%). The frequency of urethral dilation appears to have decreased over the years, with a rate of 1,170 per 100,000 in 2014 to 640 per 100,000 in 2019 (see Figure). From 2020 to 2022, there was a drastic decrease in urethral dilations, reflecting what was seen during the COVID-19 pandemic. However, these rates for female urethral dilations remain higher than published rates of male urethral stricture disease (229-627 per 100,000),6 even though evidence suggests that true urethral strictures are rarely present.2
In this analysis, we saw relatively high rates that have been steadily declining of urethral dilation in women. We hope to investigate ways to potentially improve this rate among participating practices in the AQUA registry. One potential lever is improving diversity and representation in the workforce, as female representation in the urology workforce has increased 9% per year since 2014.7 Women still represent only 10% of practicing urologists, so there is ample room for improvement.
1. Osman NI, Mangera A, Chapple CR. A systematic review of surgical techniques used in the treatment of female urethral stricture. Eur Urol. Dec 2013;64(6):965-73. doi:10.1016/j.eururo.2013.07.038
2. Santucci RA, Payne CK, Anger JT, Saigal CS, Project UDiA. Office dilation of the female urethra: a quality of care problem in the field of urology. J Urol. Nov 2008;180(5):2068-75. doi:10.1016/j.juro.2008.07.037
3. McLean P, Emmett JL. Internal urethrotomy in women for recurrent infection and chronic urethritis. J Urol. May 1969;101(5):724-8. doi:10.1016/s0022-5347(17)62411-x
4. Carson CC, Segura JW, Osborne DM. Evaluation and treatment of the female urethral syndrome. J Urol. Nov 1980;124(5):609-10. doi:10.1016/s0022-5347(17)55578-0
5. Keegan KA, Nanigian DK, Stone AR. Female urethral stricture disease. Curr Urol Rep. Sep 2008;9(5):419-23. doi:10.1007/s11934-008-0071-7
6. Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol. May 2007;177(5):1667-74. doi:10.1016/j.juro.2007.01.041
7. American Urological Association 2020 State of Urology Workforce census Book. American Urological Association; Census Results Special Report. Accessed Feb 1,2022.

Let's Accelerate Research Together
To learn more about Verana Health, please fill out the information below and our team will follow up with you as soon as possible.